Now that the family is sick, dad wants more understanding about FPRs
Cumberland County farmer Charles Barry moved from Carlisle after he said a neighboring farm made his children sick by spreading food processing residue.
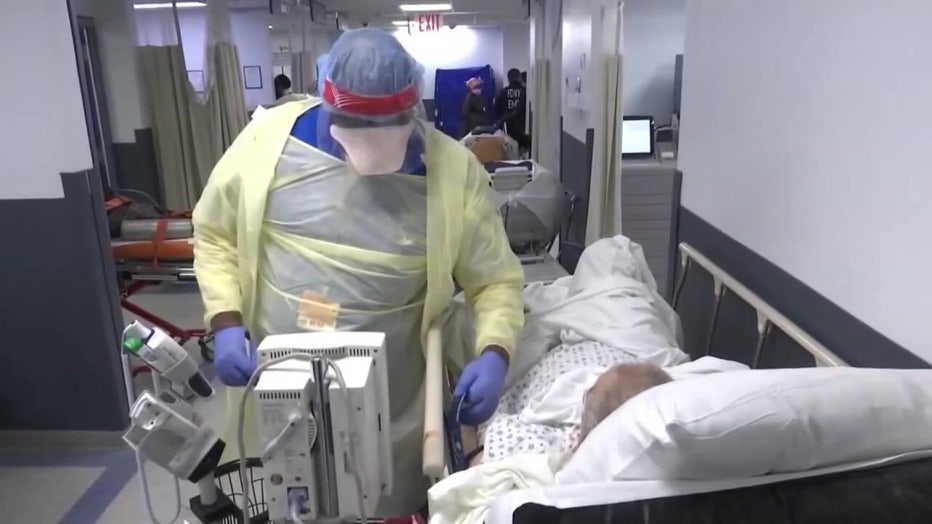
There are staff shortages in almost every area of work, and hospitals have been chronically understaffed for years.
According to Wayne Reich, CEO of the Pennsylvania State Nurses Association, Pennsylvania is currently one of the largest producers of nurses per year.
After Florida and California, the number of registered nurses in the state was 190,470.
And despite the large number of nursing graduates entering the job market, just as many are leaving the field. “Nurses come out of school, work for a few months and find out this isn’t really what they signed up for — and they leave,” Reich said.
According to Reich, hospitals are seeing a shortage of nurses who want to work at the bedside, face-to-face with patients.
Reich said the conditions at the bedside right now are such that nurses don’t want to be there.
On some occasions, new graduates will choose to go back to school and become advanced practitioners, while others leave the profession altogether, which Reich says is difficult.
In California, in an effort to expand access to more affordable Bachelor of Science in Nursing programs and fill critical nursing shortages in the state, a bill could allow several community colleges with existing two-year nursing programs to offer a four-year nursing program . .
According to the Hospital and Healthsystem Association of Pennsylvania, hospitals are working hard to recruit, retain and develop healthcare providers through higher wages, flexible schedules and tuition assistance programs.
Despite this, hospitals statewide still face an average vacancy rate of “14% for nurses and even greater challenges in rural communities.”
Pennsylvania is expected to have a shortage of more than 20,000 nurses by 2026 — the worst nationally.
‘Health care professionals are increasingly in demand’
Dr. Emmanuel B. John has worked across the country, including in California, the Midwest and Virginia, and is currently dean of the York College Nursing program. John believes that the nursing shortage is caused by several factors, and that many nurses return to school after a year or two in the field.
York College has established partnerships with local hospitals and healthcare facilities, providing students with a valuable opportunity to gain experience during their education.
Partnerships with WellSpan Health and UPMC allow students to work in real healthcare settings, allowing them to graduate as well-rounded nurses.
“We have programs in abundance, but despite the best nursing programs, there is still a shortage.” John said, adding, “A handful of students return immediately for their master’s degrees or to become nurse practitioners.”
Although both registered nurses and nurse practitioners focus on patient care and observation, NPs may prescribe treatments, order tests, and diagnose patients – tasks normally performed by physicians – while RNs are not and often work under a physician who handles patient care, diagnoses, and determines diagnoses. follow up.
York College encourages registered nurses to have two to three years of experience before returning so they can gain more experience working with patients. “There are other institutions that only require one year of experience.”
One thing that John says comes from burnout is the pressure of high expectations from hospitals.
“There is pressure on the hospital (healthcare) system, there is pressure on reimbursement rates for hospital services, and therefore healthcare professionals are increasingly being asked to do more.”
John said that healthcare professionals who provide care and services to patients and their families are also human beings, which is often overlooked. “We all have our physical limitations.”
Bad working conditions
A new study from the University of Pennsylvania School of Nursing’s Center for Health Outcomes and Policy Research finds that, next to retirements, poor working conditions are the top reason nurses leave their health care jobs.
According to the study, in various healthcare settings, including hospitals, long-term care facilities and outpatient care, planned retirement was the most commonly cited reason why nurses leave their healthcare jobs, followed by poor work-life balance and inadequate staffing, which ultimately leads to burnout.
“Nurses do not leave primarily for personal reasons, such as going back to school or because they lack resilience,” said senior author Karen Lasater. “They work in chronically understaffed conditions, which is an ongoing problem that predates the pandemic.”
Some hospitals are seeing mass layoffs
Pittsburgh-based healthcare giant UPMC announced in April of this year its plan to cut more than 1,000 jobs, many of them non-clinical, within its hospitals.
A spokesperson for UPMC said this round of layoffs will not impact bedside nurses and that staffing demands are “made based on the needs of the community.”
UPMC, which currently operates more than 40 hospitals and 800 physician practices and outpatient clinics in Pennsylvania and around the world, said the company has reduced its workforce through “non-clinical administrative workforces,” and that it will provide affected employees with better severance benefits and offers better benefits to ensure the facilities continue to thrive.
In York County, UPMC hospitals have received online feedback in recent months about complaints, including increasingly long wait times and a lack of attention and communication from nurses.
In an April statement from Paul Wood, UPMC vice president and chief communications officer, the realignment would “further UPMC’s investments in our communities, facilities, commitment to clinical care and research, strategic growth, or the provision thereof in our human resources sector , do not change.” -leading benefits.”