HIV Response: Putting People First, but Key Populations Left BehindHIV Response: Putting People First, but Key Populations Left Behind At the 25th International AIDS Conference (AIDS 2024), experts highlighted the need to prioritize the well-being of those most vulnerable to HIV, particularly key populations. However, disparities persist, with these populations often facing stigma, discrimination, and limited access to essential services. Demand and Delivery: Empowering Key Populations HIV programs that engage key populations in leadership and decision-making have proven effective in reaching the most vulnerable. Key population-led interventions have also demonstrated a high impact in service delivery. Human Rights and Prevention Advocacy Christine Stegling of UNAIDS emphasizes the importance of empowering communities to advocate for prevention at national and global levels, recognizing human rights as a crucial aspect of HIV response. Sinister Link between Funding and Healthcare Cindra Feuer raises concerns about the relationship between funding genocide and defunding healthcare, highlighting the need to address the geopolitical dimensions of HIV response. Disparities in the Asia Pacific Region Midnight Poonkasetwattana of APCOM points out the significant HIV burden in the Asia Pacific region, with key populations facing disproportionately high infection rates. Low coverage of life-saving antiretroviral therapy in many countries is also a concern. Stark Inequalities in India David Bridger of UNAIDS emphasizes the need to address the service cascade gap for key populations in India, where HIV prevalence among these groups is significantly higher than in the general population. Germany’s HIV Epidemic Trends Germany’s Ministry of Health reports that new HIV infections have largely been concentrated among gay men and other men who have sex with men, people who inject drugs, and heterosexual contacts. However, new infections among people who inject drugs and through heterosexual contact have increased in recent years. In conclusion, while the conference’s theme of “Putting people first” is a reminder of the importance of human-centered HIV response, key populations continue to face barriers to access and equity. Empowering these populations, respecting human rights, and addressing the geopolitical implications of funding are essential steps towards achieving a more equitable and effective global HIV response.
“Put people first is a reminder that the people we serve is at the very heart of our work” said Professor Sharon Lewin, International Co-Chairperson of world’s largest AIDS conference this year (25th International AIDS Conference or AIDS 2024). But when we look at the global HIV response, those people who are most at risk of the virus, are rarely receiving HIV and other health services with right, human dignity and without any stigma, discrimination or criminalization.
That is why AIDS 2024 – for the first time in the history of such conferences – is dedicated an entire pre-conference on HIV key populations on the theme: “Demand and delivery: securing rights, funding and prevention,” said Michael Ighodaro, global Director of Global Black Gay Men Connect. Key populations are not only key because of their area risk of HIV acquisition but also key because key population-led interventions have proven to be most effective in delivering quality HIV and health services. HIV programs that have genuinely engaged key populations in leadership and decision-making roles at all levels, have proven to be real game-changers when it comes to reaching-the-unreached and serving the best of quality-assured healthcare services.
Christine Stegling, UNAIDS Deputy Executive Director said: “We need to empower communities to advocate for prevention at both national and global levels. This is crucial for realizing human rights. We need to make noise (again) to ensure that addressing human rights is a crucial part of furthering biomedical interventions.”
Dr Nikolay Lunchenkov is a medical doctor who focuses on serving key populations. “Key populations are still highly stigmatized around the world including the region of my origin in Eastern Europe and Central Asia. We see more oppressive laws coming leading to limited access to HIV and other health services for key populations.”
He added: “We should not forget migration when it comes to key populations and challenges they face. I had moved myself to Germany from Russia due to oppressive and dictatorship regime that had left little space for me to develop personally. We have to consider that people move from a country to country not only because they have an option but also because they are forced to survive. This is a critical point to consider when we have a political conversation around HIV response.”
Sinister link between funding genocide and defunding healthcare
Cindra Feuer of AVAC said: “AVAC and partners had launched the Global HIV Prevention Roadmap for Key Populations which outlines a strategy for the equitable expansion and delivery of HIV prevention services to key populations globally and regionally. It introduces a critical, coordinated approach led by key populations themselves to accelerate the implementation of existing and new HIV prevention interventions.”
“We have to operationalize the key recommendations that are in this global roadmap. We are doing this in the backdrop of ever-increasing diminishing of rights, resources, and validity of science…” said Cindra.
She courageously and with unwavering integrity added that “There is inherent relationship between funding genocide and defunding healthcare. Germany is among the right-wing led countries funding genocide in Palestine. This week (at AIDS 2024 in Munich, Germany) let us talk about Palestine .” We at CNS stand with Cindra.
Key populations are being left behind in Asia Pacific region
Midnight Poonkasetwattana who comes from northeast Thailand serves as Executive Director of APCOM. “Asia Pacific region has 6.7 million people living with HIV – which is the second largest number outside of Sub-Saharan Africa. We have 300,000 new HIV infections and 150,000 AIDS-related deaths in a year in Asia Pacific region. HIV epidemic is growing in certain countries of Asia Pacific, such as: Afghanistan, Bangladesh, Fiji, Laos, Papua New Guinea, and the Philippines. Coverage of lifesaving antiretroviral therapy in many countries is very low: it is about 50% in Afghanistan, Bangladesh, Fiji, Indonesia, Iran, Mongolia, Pakistan and the Philippines.”
UNAIDS report 2023 states that “Marked inequalities and diverse epidemic trends affect progress in the HIV response in Asia and the Pacific. The HIV epidemic in the region disproportionately affects people from key populations, especially young people (15–24 years), and their sexual partners. Young people accounted for around a quarter of new HIV infections in the region in 2022. In Cambodia, Indonesia, the Lao People’s Democratic Republic, Myanmar, the Philippines and Thailand, nearly half of new HIV infections occurred among young people. Although the numbers of new HIV infections and HIV-related deaths have declined overall at the regional level since 2010, some countries have experienced an expansion of their epidemics in recent years.”
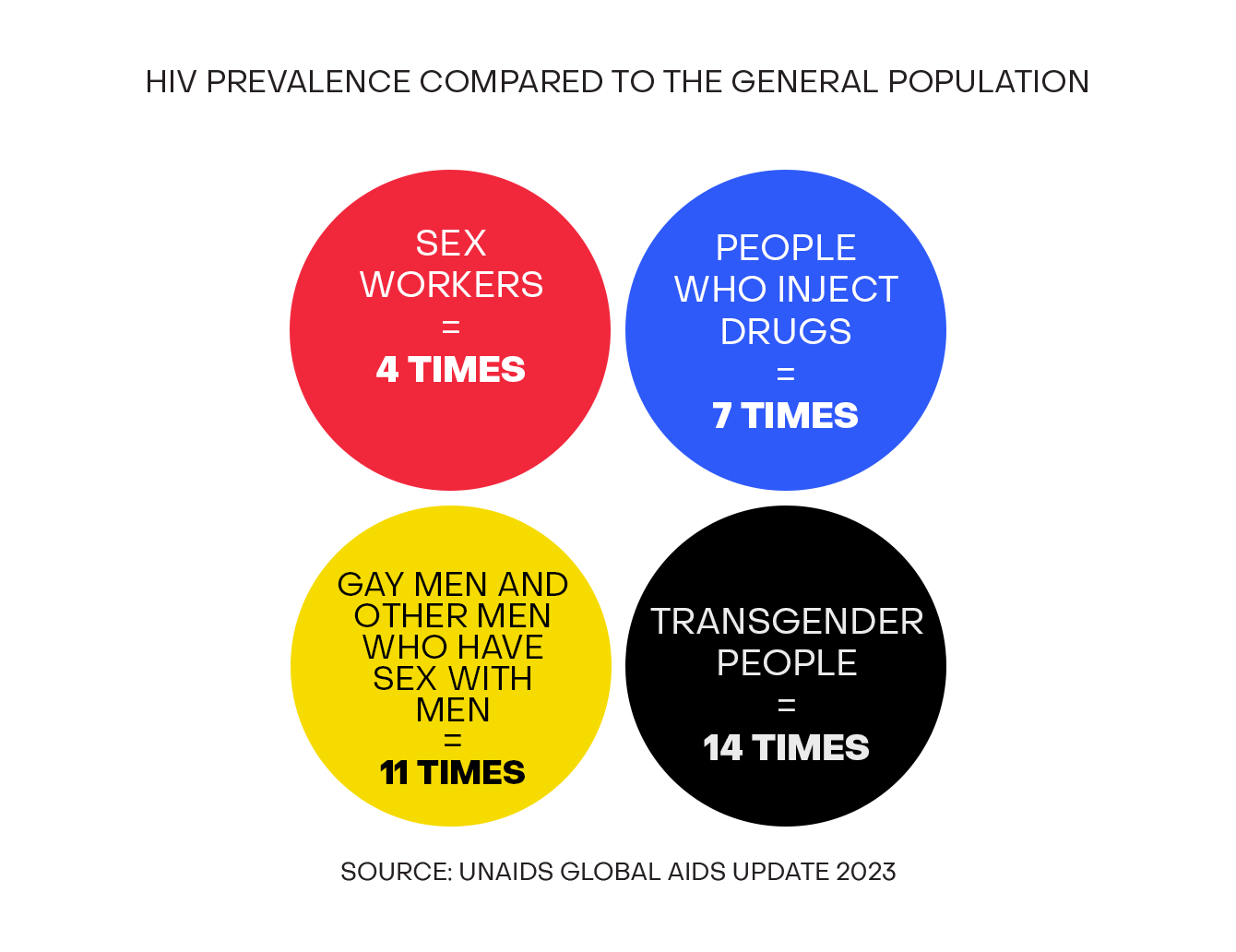
“Median HIV prevalence among people from key populations remains much higher than among the general population. Since 2010, estimated numbers of new HIV infections among gay men and other men who have sex with men increased by six times in the Philippines, tripled in Cambodia and almost doubled in the Lao People’s Democratic Republic. The increasing use of stimulants and synthetic opioids exacerbates the risks of HIV transmission among people who use drugs.”
David Bridger, UNAIDS Country Director for India said to CNS: “When we look at the HIV service cascade, key populations are lagging behind compared to general population in India. For example, among people who use and inject drugs, coverage of HIV prevention interventions is only 46%. Treatment uptake among people who use and inject drugs is also low – around 54%. HIV prevention interventions must reach all of them as it is so critical those who are currently not accessing treatment and prevention services.”
Indian government’s Sankalak report 2023 states that HIV prevalence in key populations is 9 to 43 times higher than that in general population: 1.85% among sex workers, 1.93% among inmates in prisons, 3.26% among gay men and other men who have sex with men , 3.78% among Hijra/transgender persons and 9.03% among people who inject drugs. HIV prevalence among migrant workers and truckers is 4 times than the national average of 0.20%.
Germany’s Ministry of Health told CNS that “HIV infections have remained largely confined to a few population groups, such as, gay men and other men who have sex with men, people who inject drugs, and heterosexual contacts (often among individuals from countries with high prevalence of HIV in the general population).”
“Among gay men and other men who have sex with men, the estimated number of new HIV infections in Germany has decreased from about 2,800 in 2007 to about 1,000 in 2022 (from approximately 72% to around 52% of all new HIV infections). However, among people who inject drugs, there has been a significant increase in new HIV infections – from 6% in 2010 to 20% in 2022 of all new HIV infections – with 370 new infections occurring in 2022. Infections through heterosexual contact have also shown an increasing trend in recent years, with 520 new infections in 2022 (28% of all new HIV infections in 2022)- an increase of 24% from the previous year,” said German Ministry of Health to CNS.
(Bobby Ramakant is a World Health Organization (WHO) Director General’s WNTD Awardee 2008 and serves as Health Editor at CNS (Citizen News Service). He is on the board of Global Antimicrobial Resistance Media Alliance (GAMA) and Asia Pacific Media Alliance for Health and Development (APCAT Media) Follow him on Twitter @BobbyRamakant