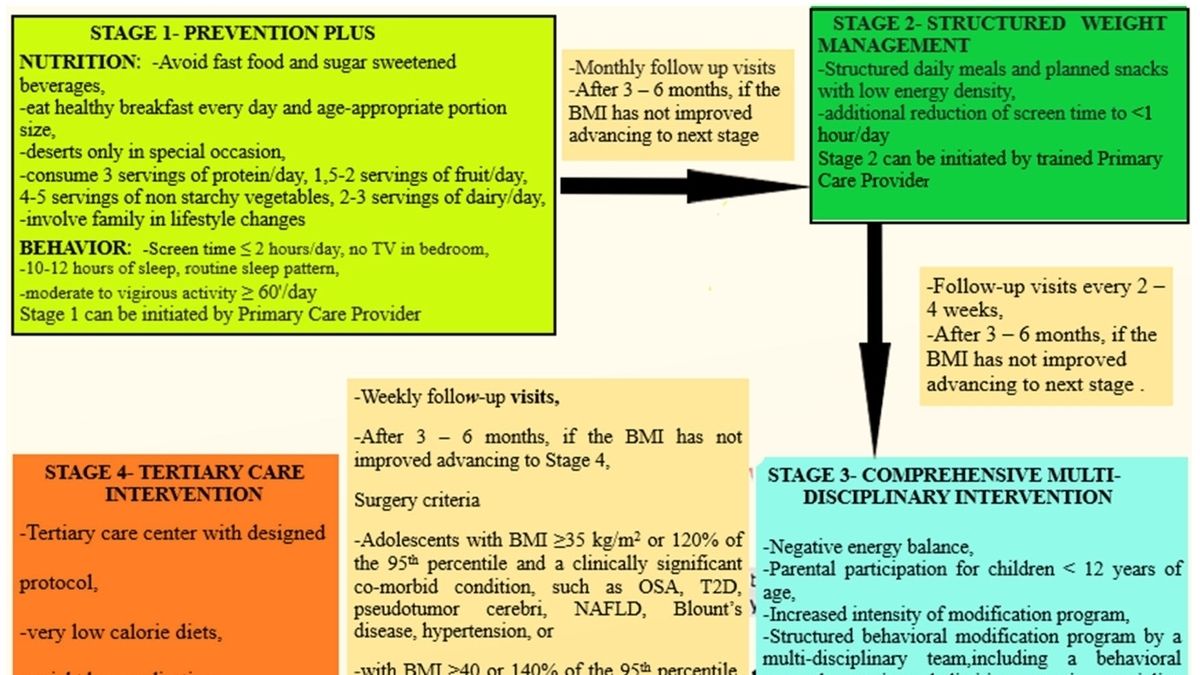
Health Panel Urges Urgent Interventions for Children and Teenagers with High BMI A prominent health panel has issued a clarion call for immediate interventions to address the alarming rise in childhood and adolescent obesity. The panel, comprised of leading medical experts and public health officials, warns that the consequences of inaction could have devastating implications for the health and well-being of future generations. According to the panel’s findings, the number of children and teenagers with a body mass index (BMI) above the 95th percentile has skyrocketed in recent decades. This excessive weight gain puts them at an increased risk of a myriad of health conditions, including: * Type 2 diabetes * High blood pressure * Heart disease * Stroke * Cancer * Mental health disorders The panel emphasizes that early intervention is crucial to prevent these devastating outcomes. They recommend a comprehensive approach that includes: * Healthy nutrition: Encouraging a balanced diet rich in fruits, vegetables, and whole grains, and limiting processed foods and sugary drinks. * Regular physical activity: Promoting daily exercise and physical activity to reduce sedentary behavior and improve overall fitness. * Behavioral counseling: Providing individualized advice and support to help children and teenagers make healthy lifestyle changes. * Medication and surgery: In extreme cases, medication or surgical interventions may be considered to assist with weight loss and improve health outcomes. The panel stresses the importance of collaboration between healthcare professionals, educators, parents, and communities to implement these interventions effectively. They call for: * School-based programs: Incorporating nutrition and physical activity into school curricula and promoting healthy eating in school cafeterias. * Community-wide initiatives: Establishing parks, recreation centers, and affordable healthy food options to create supportive environments for physical activity and healthy eating. * Parental education: Empowering parents with knowledge and skills to support their children’s healthy development. The panel urges policymakers to prioritize funding for these interventions and to implement policies that promote healthy environments for children and teenagers. By taking these steps, we can prevent the tragic consequences of childhood obesity and ensure a healthier future for our young people..
As obesity continues to loom as a major public health threat, a leading panel of independent U.S. health experts released recommendations Tuesday urging doctors to refer obese children and teens to programs that can provide advice on healthy eating, safe exercise, and understanding food labels.
.
As obesity continues to loom as a major public health threat, a leading panel of independent U.S. health experts released recommendations Tuesday urging doctors to refer obese children and teens to programs that can provide advice on healthy eating, safe exercise, and understanding food labels.
.
The U.S. Preventive Services Task Force guidelines apply to children and teens ages 6 and older with a body mass index (also called BMI) in the 95th percentile. BMI is a calculation that estimates body fat based on weight and height. The recommendations are consistent with 2017 guidelines, but the task force says it will go further and move from just screening to implementing interventions.
.
Some doctors and obesity experts are praising the efforts to address the growing crisis, but others say the task force should also consider medication interventions, including the use of a semaglutide drug, the increasingly popular class of weight loss medications. The Food and Drug Administration approved the use of the drug Wegovy in children 12 years and older in 2022.
.
“It is very important to have the option to take medication in the appropriate clinical scenario,” says Susma Vaidya, medical director at the IDEAL Clinic, the weight-loss program at Children’s National Hospital in DC. “I’m a big believer in medication, and I think we’ve been advocating for lifestyle change for a long time, but we haven’t made much progress yet.”
.
In a 2023 randomized controlled trial of semaglutide among adolescents ages 13 to 17 with a BMI at or above the 95th percentile, 44 percent of teens taking the drug recorded a drop in BMI so significant they were reclassified as normal weight or overweight. then obese.
.
But as demand for anti-obesity drugs has skyrocketed, reports of side effects including nausea, vomiting, and diarrhea have led some parents to fear that anti-obesity drugs will have long-term health consequences. Doctors respond that the physical and mental consequences of obesity can be lifelong and crippling.
.
Children who are obese are at increased risk of developing chronic conditions such as type 2 diabetes, high blood pressure, and heart disease. Obesity in childhood can have significant mental and social consequences, including depression and anxiety.
.
“We don’t have long-term data on weight loss medications, and I understand that this is concerning, but we do have long-term data on outcomes associated with obesity, and we know that people with obesity are at risk for certain comorbidities,” Vaidya said.
.
More than 19 percent of children and teens ages 2 to 19 have a BMI in the 95th percentile or higher, according to Centers for Disease Control and Prevention standards.
.
Pediatricians say adding an anti-obesity drug to a weight-loss program can significantly improve a patient’s BMI, and it’s a step that should be taken if the benefits outweigh the disadvantages.
.
“It’s a case-by-case decision based on the child, but we’re not talking about the teen who wants to lose a few pounds before the summer,” said Mona Sharifi, a pediatrician and researcher at the Yale School of Medicine and a fellow of the American Academy of Pediatrics. “We are talking about the child who has been seriously affected, and he must be presented with all his options.”
.
The task force said it did not include weight loss medications in its recommendations because the medications have not been adequately studied in adolescents. It emphasizes the importance of conducting additional research before recommending including medications in treatment plans, said John M. Ruiz, member of the U.S. Preventive Services Task Force. Recommendations or changes are typically made every five years, but as evidence about the drugs emerges, the guidelines may be adjusted, he said.
.
“If there is a fundamental change in our understanding of health challenges, the task force may sometimes revise its recommendations,” Ruiz said.
.
In contrast to the task force, the American Academy of Pediatrics recommended reviewing weight-loss medications for eligible patients with families in 2023. The biggest hurdle is getting insurers, including government programs, to cover the cost of drugs. The Medicare Modernization Act of 2003 limits coverage of weight loss medications, such as Wegovy, which can cost more than $1,000 per month without insurance.
.
The CDC estimates that childhood obesity costs the United States more than $1 billion is spent on healthcare every year. Sharifi said early interventions could reduce those costs, but added that if there is no funding for these programs, a larger group of people will need expensive drugs and surgeries later.
.
“What is heartbreaking is that despite years of recommendations showing strong evidence, we still do not have access to intensive behavioral treatment programs nationally,” Sharifi said. “There are pediatricians who try to fit these interventions into their 20-minute appointments with families, but it doesn’t work.”
Health Panel Urges Interventions for Youth with Elevated BMI A renowned health panel has issued a clarion call for immediate interventions to address the rising prevalence of high body mass index (BMI) among children and teenagers. The panel emphasized the urgent need for comprehensive strategies to promote healthy weight management and prevent obesity-related health risks. The panel’s report highlights alarming statistics indicating an alarming increase in the number of children and teenagers with elevated BMI, a measure of body fat based on height and weight. This trend poses significant health concerns, as high BMI is strongly associated with a myriad of chronic diseases, including cardiovascular disease, type 2 diabetes, and certain cancers. The panel outlined a multi-faceted plan to combat this growing crisis. The recommendations include: * Implementing school-based nutrition and physical activity programs * Educating parents and caregivers about healthy eating and exercise habits * Limiting access to unhealthy foods and beverages through policy changes * Promoting breastfeeding and reducing formula feeding * Providing affordable access to healthy food options in low-income communities The panel stressed the importance of early intervention, emphasizing that establishing healthy habits in childhood and adolescence can have profound and lasting benefits for overall health and well-being. They also emphasized the need for increased funding and research to support these critical efforts. The panel’s call to action is a timely reminder of the importance of prioritizing youth health. By investing in interventions that promote healthy weight management, we can safeguard the future health of our children and create a healthier society for all.