Misconceptions Surrounding South Africa’s National Health Insurance ActMisconceptions Surrounding South Africa’s National Health Insurance Act President Cyril Ramaphosa’s signing of the National Health Insurance (NHI) Bill into law has been met with both optimism and apprehension. While the aim of universal healthcare for all citizens is undoubtedly noble, the rhetoric leading up to the Act’s implementation has given rise to several misconceptions about the role of medical plans. Medical Schemes Remain Viable One prevalent misunderstanding is that medical schemes are unsustainable and will be phased out under the NHI. However, a report commissioned by the Board of Healthcare Funders (BHF) refutes this claim. The report shows that medical schemes have remained stable from 2005 to 2022, with an increase in beneficiaries and a solid financial position. Healthcare as a Social, Not Public, Good Another misconception is that healthcare services are a public good, meaning they should be provided by the government and accessible to everyone regardless of payment. However, the report clarifies that healthcare is more accurately described as a social good, which requires some form of payment or contribution to ensure its sustainability. Diversity in Medical Scheme Beneficiaries Furthermore, the claim that private healthcare predominantly serves the white population is unfounded. Data from Statistics SA reveals that a majority of those using private healthcare are Black African. Balanced Approach to Healthcare Reform While the BHF supports healthcare reform, it raises concerns about the constitutionality of the NHI Act. It advocates for a balanced approach that takes into account both the strengths and weaknesses of the public and private healthcare sectors. Medical schemes provide a valuable service in ensuring the viability of South Africa’s healthcare ecosystem. Informed Debate It is crucial to engage in a well-informed debate about the implications of the NHI Act. By presenting both sides of the issue, we can reach a more comprehensive understanding of the potential impact on individuals and the healthcare system as a whole. Conclusion Misconceptions about medical schemes and the role of the NHI can undermine the efforts to transform South Africa’s healthcare landscape. It is essential to base discussions on facts and evidence to ensure that the best possible outcomes are achieved for all citizens.
In an effort to transform South Africa’s healthcare landscape, President Cyril Ramaphosa signed the National Health Insurance (NHI) Bill into law.
This decision promises to move the country toward universal healthcare for all citizens, regardless of their socio-economic status.
While the purpose of UHC is laudable, the rhetoric leading up to the announcement of the NHI Act has given rise to misconceptions about the role of medical programs, with many believing that they should immediately cancel their membership in order to enjoy free healthcare in the near future to be able to enjoy.
However, the implementation of NHI will take several years.
READ ALSO | Advice | You can’t save the world
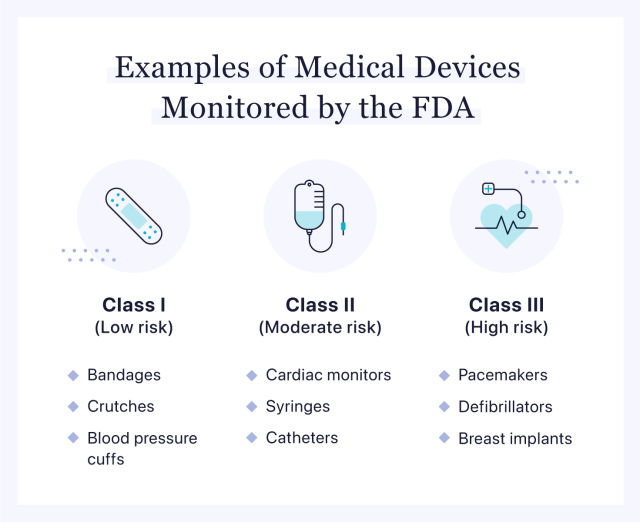
The NHI Act introduces a single-payer system. Central to the idea is that healthcare is a public good, which suggests that all healthcare financing should exclude medical schemes and be publicly funded.
However, healthcare is more accurately described as a social good.
A public good, like military services, is a good that the government must provide and from which no one can be excluded, regardless of payment. Although healthcare is essential, it is not feasible to provide it as a public good.
The Board of Healthcare Funders (BHF), concerned about the misconceptions being propagated by government representatives since 2009, has commissioned Professor Alex van den Heever, Chair of Social Security Systems Administration and Management Studies at Wits Health Consortium, to investigate these claims.
Despite their hyperbolic nature and lack of systematic research, these claims carry significant weight due to the support they receive from influential individuals.
Van den Heever’s report frequently mentions repeated statements that he concluded are untrue.
Key findings from the report
Medical plans are unsustainable – false
In 2009, claims suggested that many medical schemes were on the brink of collapse due to unsustainable funding models, with 18 schemes reportedly close to bankruptcy.
Van den Heever’s report refutes this and shows stability in medical schemes from 2005 to 2022. The number of beneficiaries increased by over 1 million between 2009 and 2022, with consolidated reserves of R114 billion in 2022, well above the required reserve ratio of 25 %. Broker costs have not been a systemic problem, and total non-health costs per average beneficiary per month for all medical schemes have fallen by 34.7% in real terms between 2005 and 2020.
Healthcare services are a public good – not true
In 2011, Health Minister Aaron Motsoaledi claimed that private healthcare is a “brutal system” due to commercialization.
READ ALSO | Police are appealing for help in identifying the woman’s body
However, Van den Heever clarified that healthcare is not a public good in an economic sense, because it does not meet the criteria of being jointly consumed without exclusion.
Healthcare is a crucial service, but offering it as a public good is not feasible.
Most beneficiaries of medical schemes are white – false
Last year, Professor Olive Shisana, honorary professor at the University of Cape Town and special advisor to Ramaphosa, stated that the private sector mainly serves the privileged white population.
However, Statistics SA’s 2021 survey shows that of all those using private healthcare, 50.2% are Black African, 32.3% White, 9.8% Colored and 7.6% Indian/Asian.
a balanced perspective
While the BHF supports healthcare reform, it raises concerns about the constitutionality of the NHI Act and calls for a factual assessment of claims about medical schemes.
It is critical to present both sides of the debate to fully understand the implications. Addressing the impact of the NHI on people could provide a more comprehensive picture.
Medical schemes are a valuable national asset that plays a critical role in ensuring the viability of South Africa’s healthcare ecosystem.
BHF advocates a balanced approach to healthcare reform, taking into account the strengths and weaknesses of the public and private sectors.
•Dr. Katlego Mothudi is director of the Board of Healthcare Funders.